iPS cell treatment: Researchers at Kyoto University conducted a successful trial to improve motor functions in Parkinson’s patients.
iPS cell treatment was tested on seven Parkinson’s patients aged 50-69.
Trial by Kyoto University’s CiRA showed improved motor functions in four patients.
No severe adverse effects reported; dopamine production confirmed in all six monitored cases.
The treatment has the potential to revolutionize Parkinson’s care pending state approval.
Introduction to Parkinson’s and iPS Cell Treatment
Parkinson’s disease, a devastating neurodegenerative disorder, affects an estimated 250,000 people in Japan alone. Characterized by the gradual decline of dopamine-producing brain cells, the disease progressively impairs patients’ motor functions, leaving many unable to perform basic movements. For decades, researchers have sought a viable solution to alleviate this condition and restore movement. The latest breakthrough comes from a clinical trial at Kyoto University’s Center for iPS Cell Research and Application (CiRA), where researchers developed and tested a revolutionary therapy involving induced pluripotent stem cells (iPS cells).
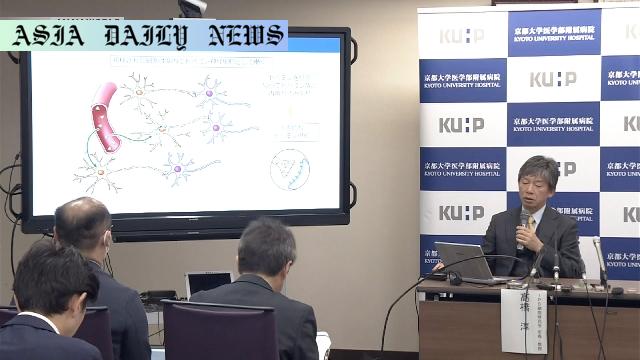
Understanding the Experiment and Its Results
The clinical trial involved seven patients aged between 50 and 69, each suffering from Parkinson’s disease. Researchers led by Professor Takahashi Jun aimed to replace the lost dopamine-producing neurons by transplanting dopaminergic cells derived from iPS cells into their brains. The therapy entailed administering either five million or 10 million dopaminergic cells per patient. These cells, famed for their adaptability, can grow into any type of body tissue. Importantly, the highly monitored trial reported no severe adverse reactions in any participant, thereby validating the safety of the treatment.
Over a two-year monitoring period, researchers were encouraged to discover that the transplanted cells produced dopamine in all six patients who completed the study. This biophysical change translated into tangible improvements in motor functions for four of the participants, reflecting the therapy’s potential effectiveness. This groundbreaking progress breathes new hope into the lives of Parkinson’s patients worldwide.
The Road to Commercialization
As promising as the results are, the path to making this therapy widely available involves several steps. The research team partnered with Sumitomo Pharma, a pharmaceutical company poised to apply for governmental approval to commercially produce the dopaminergic cells. Professor Takahashi emphasized that the ability of cell transplants to improve symptoms represents a revolutionary milestone in medical science. The ultimate objective is to offer this therapy to patients on a broader scale, but government approval must precede any large-scale treatment plans.
Implications for Parkinson’s and Future Therapies
The implications of this study extend far beyond Parkinson’s treatment. iPS cell technology could open doors to therapies for a range of neurodegenerative conditions. This demonstration of efficacy and safety lays the groundwork for new scientific endeavors aimed at addressing diseases that have traditionally been resistant to conventional treatments. The research heralds a significant scientific and medical achievement that may redefine how humanity combats progressive neurological disorders.
Conclusion
Kyoto University’s clinical trial of iPS cell-based therapy has reshaped possibilities in Parkinson’s care, showcasing a promising solution to one of the world’s most devastating neurodegenerative diseases. With no severe adverse effects and tangible improvements in four of seven trial participants, the therapy demonstrates both safety and efficacy. The announcement brings a new wave of optimism to patients, researchers, and advocates, highlighting the transformative potential of cutting-edge medical research. As stakeholders await governmental approval for large-scale commercialization, this breakthrough marks a critical turning point in the fight against Parkinson’s.
Commentary
A Landmark in Parkinson’s Treatment
The recent clinical trial conducted by Kyoto University’s CiRA marks a monumental step toward redefining Parkinson’s care. For years, this progressive disease has been synonymous with declining motor ability and compromised quality of life. However, this breakthrough offers something truly revolutionary: hope. The use of iPS cells to restore lost dopamine production validates decades of research in regenerative medicine and proves that innovative solutions can indeed tackle seemingly insurmountable medical challenges. The success story here goes far beyond the patients treated; it is about the scientific and human pursuit of better health, resilience, and dignity.
The Broader Impact of iPS Technology
The success of this trial extends beyond Parkinson’s and signals a new era in personalized medicine. iPS cells, with their ability to transform into any bodily tissue, hold the promise of addressing a variety of conditions that were previously untreatable. From spinal cord injuries to cardiovascular diseases, the adaptability of these cells could revolutionize treatment protocols across many disciplines. The research underlines the critical role of stem cell science in the evolving sphere of medicine. It’s a humbling reminder of the transformative power of human ingenuity and relentless pursuit of solutions.
The Path Ahead
Nonetheless, the achievements of this trial should not overshadow the challenges that lie ahead. From regulatory approvals to ensuring equal access for patients globally, there’s much work to be done. The involvement of key pharmaceutical players like Sumitomo Pharma indicates that commercialization could happen sooner rather than later. However, as this advanced therapy edges closer to broader availability, ethical, logistical, and financial considerations must be addressed comprehensively. The ultimate goal must be to democratize access to this innovative treatment, ensuring it becomes a beacon of hope for all patients, regardless of their circumstances.